Keratoconus is a progressive eye condition that can cause significant vision impairment. We offer a range of surgical treatments to help manage this condition, including corneal cross-linking and corneal implants, to improve our patients' vision and quality of life.
What Causes Keratoconus?
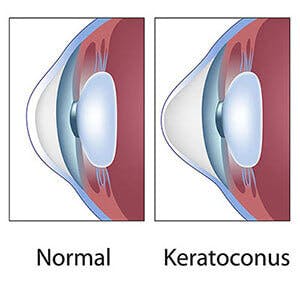
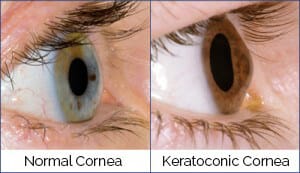
Research indicates that keratoconus may be caused by an excess of enzymes that break down the proteins within the corneal surface, causing the cornea to thin and protrude.
It is believed that keratoconus may be genetically inherited. Blood relatives of someone affected with keratoconus may either have a history of keratoconus itself or may have minor changes in their corneas that may indicate that keratoconus probably varies in both specific genetic cause, as well as in its expression within a family. Vigorous eye rubbing can contribute to the progression of the disease. People with keratoconus should avoid rubbing their eyes.